Dr Frame’s Crucial Case Notes| Dislocating Knee Caps
This month’s case study isn’t about tragedy on the slopes; rather a feel-good tale of a girl who wanted to ski but couldn’t because of issues with her knees. After a lot of work, we got her skiing!
Let’s call this person Helen. Since the age of 10 Helen had knee problems. In PE at school she had dislocating knee caps – not as rare as you might think. Sometimes it happens after an injury where the knee cap is forced out of the groove it runs in and stretches all the structures holding it in. As these structures no longer function in helping to guide the knee cap, it can keep dislocating. For example, I have patients who have been hit in a tackle playing rugby that dislocates their patella. Most get back to normal with rest and physio but a few (usually the older ones) go on to dislocate recurrently.
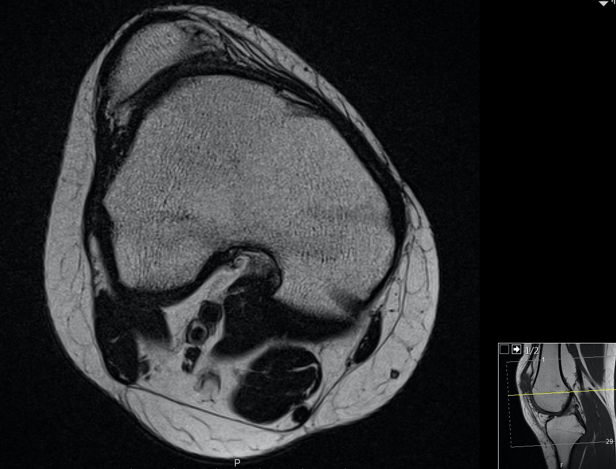
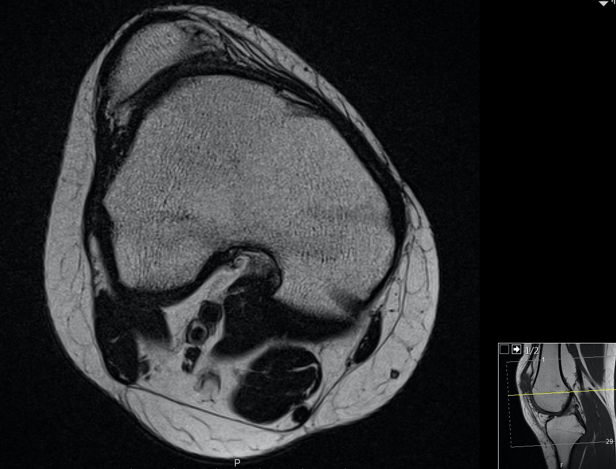
Helen’s dislocation happened without a specific injury. This is most commonly found in young girls who are hypermobile (with very stretchy, elastic ligaments and tendons), who have a family history of knee cap problems, knock knees and in toeing (internal rotation of the feet). Helen had all these and worse. When we scanned her knees she had no groove at all for her knee cap to run in, so even dashing for a train or getting out of bed too fast meant her knee caps dislocated. She was desperate to live life fully and felt jealous of her friends at university who were having fun skiing.
We set off on a year-long course of multiple surgeries. First we did a de-rotation osteotomy to correct the amount her femurs (thigh bones) were turned in. We made a controlled break in the bone above her knee and turned her leg nearly 30°. This was held with a carbon fibre-reinforced plate and screws in the bone. After two to three months we went back in to complete the surgery.
We had to make a new groove for her knee cap to run in. This is complex surgery called a trochleoplasty. We created a new knee shape by removing bone under the smooth shiny cartilage then pushing the surface above into this new shape and holding it there to heal. We also did a ligament reconstruction to recreate the structure stretched when the knee cap had dislocated in the past. Finally, we took the attachment of her patellar tendon where it attaches onto the shin bone and moved it to allow the knee cap in its new groove to run in a straight line.
Helen brushed off this two-hour complex surgery with surprising ease. Just two months later her wounds had healed, her knee was bending well and her knee cap was stable and moving normally. No more dislocations, no more thinking about how to move. Although it was a long process, the results are amazing. It makes my job feel so worthwhile when I see motivated, resilient people make incredible recoveries.
A year on from her first surgery and after lots of hard work and physio, Helen went skiing. She sent me pictures of her snowploughing down her first blue – something she though would never be possible. Well done Helen!
Mr Mark Frame MBChB MRCS FRSC is a trauma and knee surgeon at the University Hospital Southampton/Spire Hospital Southampton.